
In today’s healthcare landscape, the need for accessible and quality medical services is more pronounced than ever. Shortages of physicians and other key members of the healthcare workforce are impacting states across the country.
Access to healthcare can be defined as the ability to obtain healthcare services such as prevention, diagnosis, treatment, and management of diseases, illness, disorders, and other health-impacting conditions.
As the demand for healthcare services continues to rise, the role of advanced practice providers becomes increasingly vital in bridging the healthcare gap.
In this post, we explore the importance of Physician Assistants (PAs), also known as Physician Associates, in expanding healthcare access within the United States, shedding light on their unique contributions and the challenges they face in meeting the growing healthcare demands.
Research on Healthcare Access
The United States faces a multitude of healthcare challenges, from an aging population to the increasing prevalence of chronic diseases. These factors, coupled with a shortage of primary care physicians and a lack of adequate healthcare infrastructure in many areas, contributes to the strain on the healthcare system. As the demand for medical services escalates, finding innovative solutions to address this gap becomes imperative.
In 2021, GoodRx Research found that over 80% of counties across the US lack proper access to the services needed to maintain health. According to the report, “over a third of the U.S. population lives in a county where there is less than adequate access to pharmacies, primary care providers, hospitals, trauma centers, and/or low-cost health centers.”
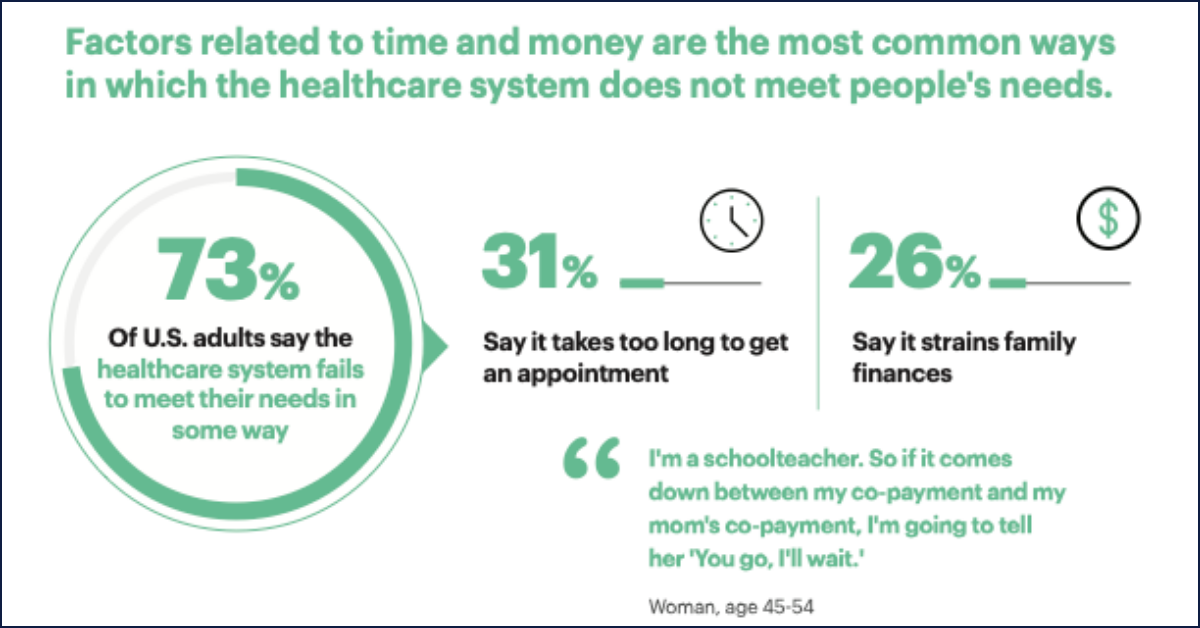
Furthermore, studies have shown other problems – long waiting times, high costs, poor patient experiences – occur as a byproduct of infrastructural deficiencies and healthcare worker shortages. Research conducted by The Harris Poll and the American Academy of Physician Associates (AAPA) found that 56% of adults wait more than a week for an appointment and 65% say that coordinating and managing healthcare is overwhelming and time-consuming. In addition, concern over cost is the top reason cited for skipping or delaying healthcare.
What Is a Physician Assistant?
A Physician Assistant (PA) is a highly trained healthcare professional who practices medicine. Depending on state regulations, sometimes Physician Assistants practice in collaboration with a licensed physician.
According to the AAPA, the PA profession was established in 1967 and “currently has more than 168,300 practitioners in the US, engaging in more than 500 million patient interactions each year.”
To become a licensed Physician Assistant, individuals typically undergo a rigorous educational and clinical training process. This usually involves completing a bachelor’s degree with a focus on pre-medical or science-related coursework, followed by enrollment in a Master’s-level Physician Assistant program accredited by the Accreditation Review Commission on Education for the Physician Assistant (ARC-PA). These programs encompass both classroom education and clinical rotations, allowing PAs to gain hands-on experience in diverse medical specialties.
Upon graduation, aspiring PAs must pass the Physician Assistant National Certifying Exam (PANCE), a comprehensive assessment evaluating their medical knowledge and clinical skills. Successful completion of the PANCE qualifies individuals for state licensure, and they must adhere to state-specific regulations governing their scope of practice.
Once licensed, Physician Assistants collaborate with physicians and other healthcare professionals, providing crucial support to deliver care to patients across various healthcare settings.
Bridging the Gap: How Do Physician Assistants Expand Healthcare Access?
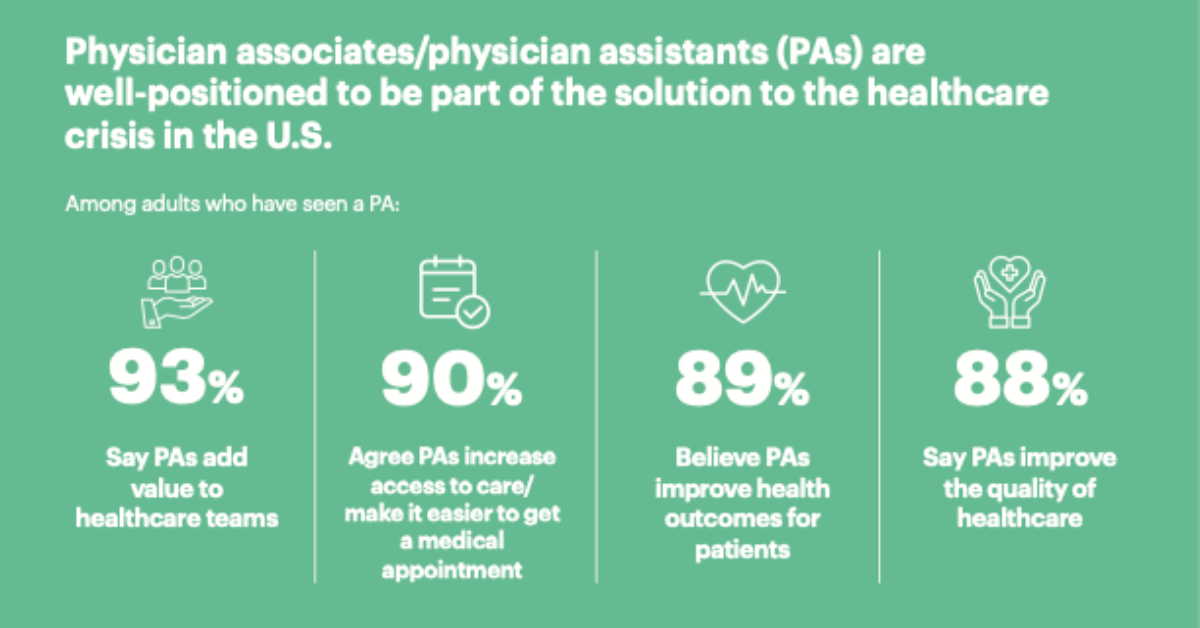
Physician Assistants have emerged as an important force in bridging the healthcare gap. First, their extensive training makes them extremely versatile. They are also capable of providing face-to-face or virtual care in underserved areas. In addition, they can provide a high-quality patient experience that an increasing number of Americans feel is lacking in today’s healthcare system.
To gain further context on this subject, we spoke to Desmond Watt, MMS, PA-C, practicing Physician Assistant and PA advocate, about the ways that PAs can positively contribute to healthcare access around the country.
Physician Shortage and Increased Access to Primary Care
In areas that are suffering from critical healthcare worker shortages, Watt cited the simple mathematics of the situation.
“What are the average wait times to see a physician in the United States – 28 days for an initial visit with a primary care physician,” said Watt. “In some cases, it’s literally a matter of the number of trained clinicians versus the number of patients. Expanding access to patient care by way of PAs as an entry point can dramatically accelerate that timeframe.”
One major contribution of Physician Assistants is their role in providing increased access to primary care. With a focus on preventive care and early intervention, PAs can help manage and treat a variety of health issues, reducing the burden on primary care physicians.
According to the National Commission on Certification of Physician Assistants (NCCPA), 34% of practicing Certified PAs indicate they have a patient panel for which they are the primary provider.
Versatility
Depending on the state in which they practice, PAs can provide a wide range of healthcare services, including diagnosing and treating illnesses, prescribing medications, and assisting in surgeries.
“One of the things that PAs do that is very unique,” said Watt, “is that we have the ability to move across specialties over the course of our career. For example, I can specialize in Cardiology for five years and then move into primary care, but I can bring that knowledge with me.”
Physician Assistants’ adaptability and versatility make them valuable assets in a healthcare system that is grappling with an expanding demand for services.
Serving Underserved Communities
Underserved communities often face barriers to healthcare access, such as geographic isolation, economic challenges, and a shortage of healthcare providers. PAs can serve as primary care providers in underserved regions, bringing much-needed medical attention to those who might otherwise lack access to healthcare services.
“When you compare to physicians, a larger rate of physician assistants and nurse practitioners tend to work in rural or care desert areas,” Watt said.
According to the Agency for Healthcare Research and Quality: “NPs and PAs are more likely than physicians to work in rural areas (16% vs. 11%), and primary care NPs and PAs are much more likely to be rural (28% and 25%, respectively). This rural distribution is higher than that of primary care physicians as a whole and similar to that of family physicians (22%).”

Telemedicine and Virtual Care
Although the use of telemedicine and virtual care was accelerated by the pandemic, healthcare has been gradually trending in this direction for many years.
Telemedicine allows patients to receive medical care from the comfort of their own homes, eliminating the need for travel and reducing wait times. This is especially beneficial for patients in rural or underserved areas who may not have easy access to healthcare facilities.
Watt firmly believes that the expansion of telehealth is a critical element in addressing the enormous challenges within the modern healthcare system. In 2018, he co-founded the AAPA special interest group PAs in Virtual Medicine and Telemedicine (PAVMT), serving as its first executive board president.
“I’ve been including virtual care as a component of my practice for nearly a decade,” said Watt. “Starting PAVMT happened as a result of looking around and realizing that, although myself and other PAs were doing virtual care work within my organization, we didn’t hear many PAs talking about it elsewhere. PAVMT focuses on the premise that PAs should be aware of practice using virtual care and telemedicine, whether or not it’s something they are participating in actively right now, because it’s here to stay.”
Collaborative Care Models
The collaborative care model, where PAs work closely with physicians and other healthcare professionals, is a key aspect of their contribution to expanding healthcare access.
At its best, the collaborative model allows for more efficient and effective patient care, as PAs can share responsibilities with physicians, thereby increasing the overall capacity of the healthcare team. Collaboration can not only enhance quality of care but also ensure that patients receive timely and comprehensive attention.
Challenges Faced by Physician Assistants
While Physician Assistants play a pivotal role in expanding healthcare access, they are not without their challenges. Further discussion and awareness of these hurdles is crucial to fully understand the potential of PAs and establish a clear pathway to meeting the nation’s healthcare needs.
Scope of Practice Restrictions
Scope of practice regulations can vary significantly from state to state, impacting the ability of PAs to provide certain services independently depending on where they practice.
Some states have more restrictive regulations, limiting the autonomy of PAs in areas such as prescribing medications or ordering diagnostic tests. PA advocates feel that addressing these inconsistencies and advocating for standardized scopes of practice can empower PAs to better contribute to healthcare access.
Watt frequently advocates for improvements to PA scope of practice legislation across the US, and he notes that collaboration is evolving to be more flexible at the practice level.
“We’ve seen some states that have made progress on legislation that allows a PA scope of practice and collaboration requirements to be defined more flexibly in the context of their practice and healthcare system needs,” Watt said. “This is a good way to enable the skills that PAs bring to patient care.”
Public Awareness and Acceptance
Despite the growing importance of Physician Assistants in healthcare, an argument could be made that there is still a need for increased public awareness and acceptance of their role.
Many individuals may not fully understand the role and capabilities of PAs, leading to misconceptions about the quality of care they can provide. Ongoing advocacy efforts focused on educating the public about the training, expertise, and contributions of PAs can help foster greater acceptance and utilization of their services.
The Future of Physician Assistants in Expanding Healthcare Access
As the landscape of healthcare continues to evolve, the role of Physician Assistants will remain important. Addressing the challenges they face and leveraging their unique skill set is essential to fully harness their potential in expanding healthcare access across the United States.
Strengthening Healthcare Collaborations
Building a healthcare system that values and prioritizes interprofessional collaboration is key to maximizing the impact of Physician Assistants. Initiatives that promote teamwork, communication, and mutual respect among healthcare professionals create an environment where PAs can contribute their unique skills and perspectives to the benefit of patient care.
This collaborative approach can be particularly important in addressing complex medical cases and ensuring comprehensive patient management.
While Watt largely advocates for an expanded scope of practice for physician assistants, he recognizes the importance of collaboration for “support, collegiality, partnership, and learning.”
“There is a value in collaboration unto itself, rather than adhering to some explicit state requirement” said Watt. “I want to talk about clinicians actually learning from each other to better support their patients.”
Conclusion
Physician Assistants are indispensable contributors to expanding healthcare access in the United States. Their ability to provide primary care in person and via telemedicine, serve underserved communities, and participate in collaborative care models positions them as vital members of the healthcare workforce. More discussion from all interested parties regarding the challenges they face, such as scope of practice restrictions and public awareness, could prove essential for fully unlocking their potential.
By embracing these measures, the healthcare system can ensure that PAs play an even more significant role in meeting the diverse and growing healthcare needs of the American population. In doing so, the United States can move towards a more accessible, efficient, and patient-centered healthcare system.