Healthcare startups and organizations looking to scale their workforces with nurse practitioners (NP) face a major operational hurdle: navigating the web of state-specific NP and physician collaboration laws. These laws—which vary dramatically across jurisdictions—dictate how NPs may practice, prescribe, and engage in patient care in collaboration with physicians.
For digital health companies, these regulations are mission-critical. Failure to comply can delay market entry, increase legal exposure, and break down trust with providers and patients. But with the right tools, knowledge, and partners, you can transform this regulatory complexity into a strategic advantage.
This guide unpacks what collaboration laws entail, how they differ by state, and how digital health companies can build compliance into their expansion strategy from day one.
Why Healthcare Collaboration Laws Matter
In many states, nurse practitioners must enter into formal collaborative agreements with physicians to diagnose, treat, and prescribe. These agreements often involve specific requirements governed by state law, such as:
-
Defined scopes of responsibility
-
Regular chart reviews
-
Scheduled meetings or case conferences
-
Oversight of prescribing practices
-
Documentation and board submissions
Noncompliance with these laws can lead to delayed market entry, license sanctions, or worse—patient safety risks. That’s why forward-thinking digital health companies are building compliance into their operational models from the start.
State laws may also cap how many NPs a single physician can collaborate with, impose transition periods before independent practice is permitted, and require board approval before services can begin. Each of these elements creates friction that can slow down your expansion unless addressed head-on.
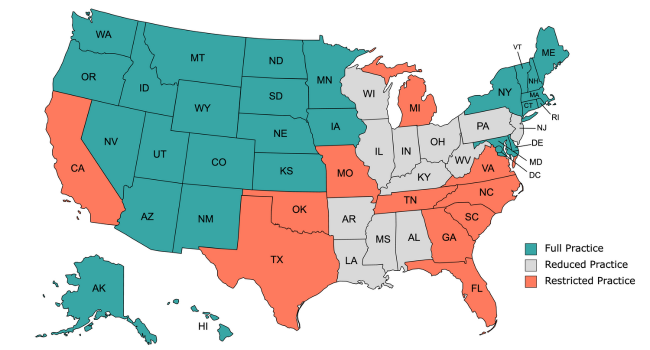
NP Practice Authority: Full, Reduced, or Restricted?
States fall into three general categories of NP practice authority.
Full Practice
NPs can evaluate patients, diagnose, interpret tests, and initiate treatments—including prescribing—without physician oversight (e.g., Arizona, Oregon, Washington). Full-practice states are the most straightforward environments for scaling digital health operations. However, even here, clinical governance and payer-specific rules still apply, so oversight infrastructure is still essential.
Reduced Practice
NPs can practice independently but must have a formal agreement for one or more elements of care (e.g., Arkansas, Ohio). Sometimes, these states have transitional independence models, where NPs can gain autonomy after a certain number of hours or years working in a collaborative model.
Restricted Practice
NPs must work under physician supervision for the entirety of care delivery and prescribing (e.g., Alabama, Texas, Georgia). For digital health companies, restricted-practice states present the greatest challenges. Many require pre-approved documentation, specific NP-to-physician ratios, and defined geographic proximity.
These classifications are the foundation for understanding compliance—but it only scratches the surface.
State-Specific Barriers: Independence, Filings & Ratios
Here’s how the complexity deepens:
1. Transition To Independence Requirements
Some states, like California and Arkansas, offer “transition to independence” pathways—meaning NPs must work under supervision for a certain number of hours or years before practicing solo. For instance, California mandates 9,200 hours or six full-time equivalent years before independence is granted.
2. Board Submission & Approval Delays
Even if collaboration agreements are executed, NPs in states like Alabama and Arkansas cannot practice until the board approves the relationship, which can take over 60 days in some cases.
Failure to wait for approval can result in fines, disciplinary action, or suspension of the collaboration agreement. These delays can severely impact hiring, credentialing, and onboarding timelines. Automating board submission tracking is essential for mitigating this bottleneck.
3. NP-to-Physician Ratios
Several states place caps on how many NPs a physician may collaborate with. For example:
-
Alabama: 1 physician per 9 FTE NPs
-
California: 1 physician per 4 NPs
-
Georgia: Capped collaborative capacity with added geographic restrictions
These rules present a major constraint on scaling a digital provider network. Companies that don’t proactively manage capacity and match NPs to appropriately credentialed physicians risk breaching state law and compromising patient safety.

The Georgia Example: Navigating Collaboration Complexity at Scale
Let’s take a closer look at Georgia, one of the most challenging states for NP-physician collaboration:
-
Geographic Proximity Required: Collaborating physicians must be actively practicing in Georgia.
-
Supervision Ratio: One physician can collaborate with no more than 8 NPs.
-
Annual On-Site Meeting: The collaborating physician must coordinate and attend an in-person session each year.
-
Board Approval Required: All collaboration protocols must be submitted and approved by the board before clinical work begins.
-
Ongoing QA: Physicians must review 10% of patient charts and conduct quarterly quality assessments.
These overlapping requirements make compliance labor-intensive and prone to error—unless your organization partners with a platform like Zivian Health that automates and streamlines these processes.
Best Practices for Digital Health Compliance
Automate Regulatory Intelligence
Use tools like Zivian Health’s Compliance Rules Engine to dynamically track and enforce collaboration rules by state—including required documentation, ratios, and board filing deadlines.
Centralize Collaboration Agreements
Digitally manage and store all collaboration agreements, workflows, and communication to create a defensible audit trail for all stakeholders.
Use a Nationwide Physician Network
To streamline onboarding, work with a platform that can instantly match NPs with vetted physicians who meet clinical and state regulatory requirements.
Scaling Compliance Across State Lines with Zivian Health
Zivian Health helps digital health organizations simplify multi-state expansion by automating NP-physician collaborations, tracking real-time compliance, and reducing operational friction. With expertise in challenging regulatory environments like Georgia, Mississippi, and South Carolina, Zivian turns compliance into a growth enabler—not a blocker.
Navigating the patchwork of NP-physician collaboration laws is no small feat—but it’s an important task for digital health companies scaling across state lines. By understanding each state’s requirements and implementing smart, automated compliance strategies, organizations can unlock new markets faster and with confidence.
Need help scaling your clinical workforce compliantly? Connect with Zivian Health today and turn regulatory complexity into competitive advantage.