
Nurse practitioners (NPs) have moved from supportive roles to the center of care delivery. But despite their growing role, one factor still defines where and how NPs can practice: state-level practice authority laws.
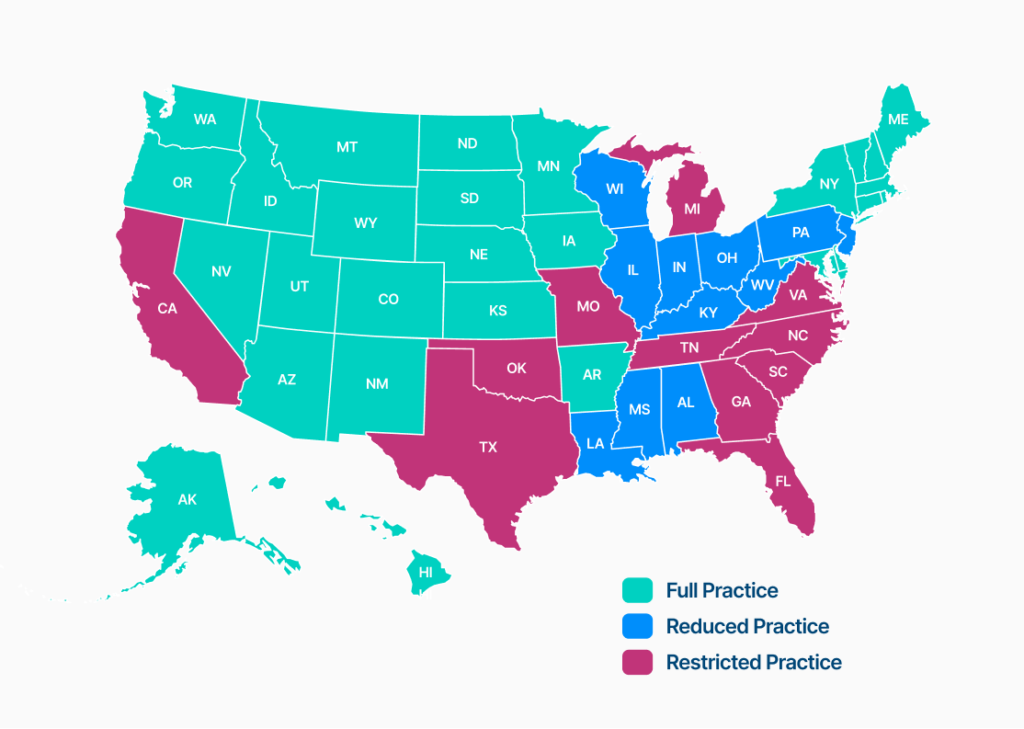
NP practice authority determines the level of autonomy a nurse practitioner has to evaluate patients, diagnose conditions, prescribe medications, and manage care. Each state defines and enforces one of three practice authority models:
-
Restricted Practice Authority
-
Reduced Practice Authority
-
Full Practice Authority
Understanding these distinctions is important for NPs planning their careers and healthcare organizations scaling across state lines.
Below, we break down each type of practice environment, including the real-world pros, cons, and compliance implications.
What Is Nurse Practitioner Practice Authority?
Practice authority refers to the legal framework that dictates how independently a nurse practitioner can practice medicine within a given state. These laws are set at the state level and influence:
-
Whether physician collaboration or supervision is required
-
Prescriptive authority and medication limitations
-
Chart review, meeting, and documentation requirements
-
Speed of workforce activation and onboarding
For healthcare organizations operating in multiple states, these laws can introduce operational complexity that must be actively managed to remain compliant.
Restricted Practice Authority
Restricted Practice Authority represents the most limiting model for nurse practitioners. In these states, NPs are required to practice under direct physician supervision for all aspects of patient care, including patient evaluation, diagnosis, treatment decisions, and prescribing.
Physician oversight is a continuous legal requirement that governs both clinical decision-making and operational workflows. Supervising physicians are typically responsible for chart review, availability for consultation, and formal documentation of oversight activities.
Pros of Restricted Practice Authority
Structured Supervision and Mentorship
Direct physician oversight can provide clinical support for early-career NPs, particularly in complex specialties.
Team-Based Care Models
These environments emphasize close collaboration, which can support continuity and shared decision-making when workflows are well designed.
Cons of Restricted Practice Authority
Limited Clinical Autonomy
NPs cannot practice to the full extent of their education and training, which can limit professional satisfaction and slow care delivery.
Operational Bottlenecks
Care delivery may be delayed when physician availability becomes an issue, which is especially problematic in rural or high-demand settings.
Scaling Challenges for Organizations
Restricted states often impose NP-to-physician ratios, board approval requirements, and ongoing documentation hurdles that complicate hiring and expansion.
Reduced Practice Authority
Reduced Practice Authority offers nurse practitioners greater independence than restricted models, but still requires a formal collaborative agreement with a physician for certain aspects of care.
In these states, NPs can independently evaluate patients, diagnose conditions, and manage treatment plans. State law or board regulation may still require physician involvement for prescribing authority, chart review, quality assurance activities, or other defined clinical functions.
The scope of collaboration varies widely by state, making reduced-practice environments operationally nuanced and highly dependent on accurate legal interpretation.
Pros of Reduced Practice Authority
Meaningful Autonomy with Clinical Support
NPs can operate independently day-to-day while retaining access to physician consultation when needed.
Flexible Collaboration Models
When structured correctly, reduced-practice environments can support efficient, team-based care without micromanagement.
Cons of Reduced Practice Authority
Prescribing and Scope Limitations
Many reduced-practice states impose restrictions on controlled substances or specialty care, which can complicate care delivery.
Compliance Complexity
Chart reviews, meeting attestations, and board filings must be carefully tracked. Missed documentation can create audit risk even when care itself is high quality.
Full Practice Authority
Full Practice Authority allows nurse practitioners to evaluate patients, diagnose conditions, interpret diagnostic tests, and prescribe medications independently without physician supervision or mandatory collaborative agreements. In full practice states, NPs are regulated solely by state nursing boards and are legally authorized to practice to the full extent of their clinical training.
As of 2026, more than half of U.S. states grant full practice authority to NPs.
However, many states impose a “transition to independence” pathway that requires newly licensed or out-of-state NPs to complete a defined period of supervised or collaborative practice before they achieve full autonomy. States typically measure these transition periods in clinical hours or years of practice and require documentation, physician attestations, or formal board approval. Although policymakers often design transition-to-independence models to support safe onboarding and clinical readiness, these frameworks introduce meaningful operational complexity.
NPs and organizations must track hours, maintain compliant collaboration agreements during the transition period, and ensure timely filings to avoid delays in full practice activation.
Pros of Full Practice Authority
Maximum Clinical Autonomy
NPs can practice to the full scope of their training, enabling faster, more responsive care.
Easier Access to Care
Full Practice Authority can increase patient access in rural and underserved areas, where physician shortages are most severe.
Operational Efficiency
Healthcare organizations can onboard and deploy NPs more quickly, without supervision-related delays.
Cons of Full Practice Authority
Increased Professional Responsibility
With autonomy comes heightened accountability. NPs must stay informed about licensure, prescribing rules, and payer requirements.
Why Ongoing Compliance Matters
Even within the same authority category, states differ widely in their requirements. Some offer transition-to-independence pathways, others impose prescribing nuances, and many update regulations frequently.
For NPs and healthcare organizations, this means:
-
A care model that is compliant in one state may be non-compliant in another
-
Manual tracking of collaboration requirements does not scale
-
Missing documentation can derail audits, payer enrollment, or expansion plans
Practice authority laws are nuanced, evolving, and require active management.
How Zivian Health Helps Nurse Practitioners and Organizations Navigate Practice Authority
At Zivian Health, we built our platform to eliminate the regulatory friction that holds NPs and healthcare organizations back.
We help nurse practitioners and healthcare organizations:
-
Navigate state-specific collaboration and practice authority laws
-
Match with vetted collaborating physicians when required
-
Automate tracking of meetings, chart reviews, and board filings
-
Maintain continuous, audit-ready compliance across all states
Instead of juggling spreadsheets, email chains, and loose documents, NPs and organizations can use Zivian as a single source of truth for workforce compliance.
Build Your Career and Your Care Model with Zivian Health
Identifying whether a state follows restricted, reduced, or full practice authority is only the first step. The real challenge is operationalizing compliance in a way that supports growth, protects clinicians, and expands patient access.
Zivian Health exists to make that possible.
If you’re a nurse practitioner navigating practice authority—or a healthcare organization scaling an APP-led workforce—we’re here to help.
Connect with Zivian Health today to get started.