The Best States for Nurse Practitioners: A Guide to NP Autonomy
Nurse practitioners (NPs) have emerged as crucial providers of primary and specialty care in the current healthcare landscape. They play a vital role in delivering quality care and filling gaps in underserved areas of the United States.
Many NPs do this within a larger health system. Others, however, want to venture out on their own. If this resonates with you, this blog post is for you!
Let's explore the best states for nurse practitioners seeking professional freedom. We’ll break down all you need to know about NP autonomy and the practice environment of every U.S. state.
Understanding NP Autonomy
NP autonomy is the extent to which nurse practitioners (NPs) can practice independently, make clinical decisions, and provide care without the direct oversight of a physician. This is often referred to as “practice authority.”
Many NPs desire autonomy — to fully utilize their advanced education, training, and clinical expertise with professional freedom. After all, NPs help increase access to care, improve health outcomes, and reduce healthcare costs in the U.S. In an effort to standardize care, however, many states have laws and regulations that restrict how the NP can practice.
This is why it is crucial to understand np supervision requirements by states in which you intend to practice.
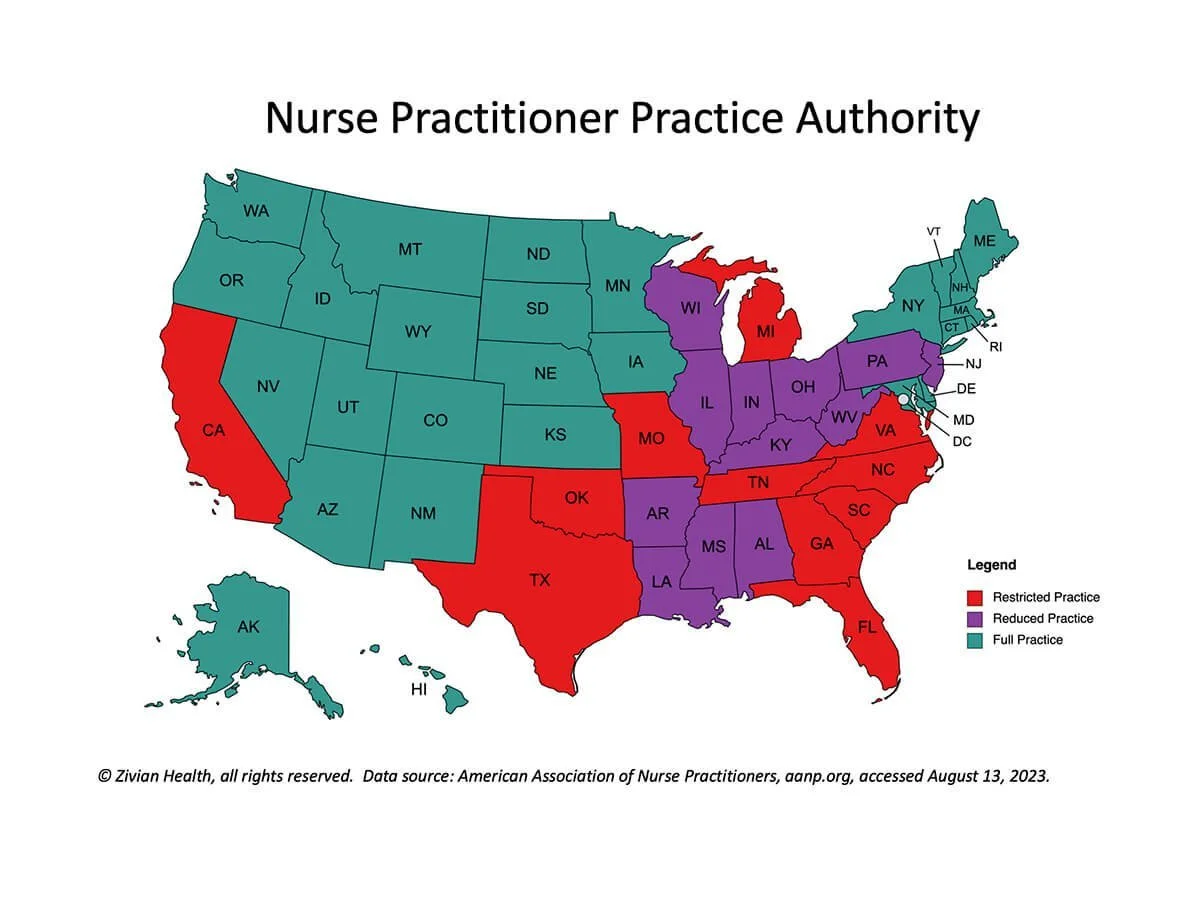
The levels of NP autonomy fall into three broad categories:
Full practice authority
Reduced practice authority, and
Restricted practice authority.
Let’s dive in, review each category, and define which states give NPs the greatest independence.
Nurse Practitioner Full Practice States
Full practice states are states where nurse practitioners practice independently without physician oversight. They are considered the best states for nurse practitioners. In these states, NPs have full authority to:
Evaluate patients
Diagnose and treat conditions
Order and interpret diagnostic tests
Make referrals to specialists, and
Prescribe medications, including controlled substances.
Full practice, in essence, means full autonomy. The NP has the authority to provide care without a supervising physician. The NP's state board of nursing exclusively grants them this authority.
Full practice states are sometimes referred to as "NP independent practice states.” This is because NPs have the most freedom in these states to establish their own practices. So it is no wonder that NPs seek to practice in these nurse practitioner-friendly states. With full autonomy, NPs feel empowered to use their unique skills and meet the healthcare demands of their communities.
Full Practice States List
Note: Several of these states are labeled as “Transition to Practice” by the American Nurses Association. This means full practice authority is gained after a set number of hours of supervised practice. We’ve noted these states with an asterisk (*) below.
Alaska
Arizona
Colorado*
To gain full prescriptive authority, Colorado requires NPs to complete 750 hours of mentorship under a physician or APRN with full practice authority.
Connecticut*
In Connecticut, a CNP or CNS must have a collaborative agreement in place with a physician and complete 3 Years and 2,000 hours of supervision before gaining full practice authority.
Delaware*
In Delaware, a CNP, CNS, CNM, or CRNA must have a collaborative agreement with a hospital or integrated clinical setting. They also must complete 2 years and 4,000 full-time hours of supervised practice before they can gain full practice authority.
Hawaii
Iowa
Idaho
Kansas
Maine*
In Maine, NPs are required to have a collaborator for their first 4,000 practicing hours.
Massachusetts*
In Massachusetts, an NP, Psychiatric CNS, or CRNA must complete 2 years of supervision under a qualified practitioner before they can gain full practice authority.
Maryland*
In Maryland, a CNP can gain full practice authority after completing 18 months of practice under the supervision of a physician or CNP mentor with 3+ years experience.
Minnesota*
In Minnesota, a CNP or CNS must have a collaborative agreement in place with an APRN or physician and complete 2,080 hours before gaining full practice authority.
Montana
Nebraska*
In Nebraska, CNPs must complete 2,000 hours of supervised practice with an MD, DO, or NP before they can gain full practice authority.
Nevada*
In Nevada, CNP, CNS, and CNMs must complete 2 years or 2,000 hours of supervised practice before they gain full prescriptive authority.
New Hampshire
New Mexico
New York*
In New York, a CNP must have a collaborating agreement with a physician and complete 3,600 hours of supervision before they can gain full practice authority.
North Dakota
Oregon
Rhode Island
South Dakota
Utah*
Vermont
In Vermont, a CNP, CNS, CNM, or CRNA must complete 24 months and 2,400 hours of supervised practice with an APRN or physician before they can gain full practice authority.
Washington
Washington, D.C.
Wyoming
Physician Collaboration in Full Practice States
Full practice gives an NP the freedom to practice without the oversight of a physician. And for this reason, you may feel they are the best states for nurse practitioners.
But many NPs still find value in hiring a collaborating physician. From having extra support to reducing risk, a collaborating physician can be worth the cost no matter where you practice.
Another important reason a full-practice NP may still seek a collaborator is for insurance credentialing. Some health payors have supervision requirements even though the state they practice in does not.
So why panel with these insurers? Because insurance is a critical component of access to care for many patients. Hiring a collaborating physician may feel like losing some of your independence, but accepting insurance can help you grow your patient population and provide care that doesn’t break the bank.
Nurse Practitioner Reduced Practice States
The next category of states are called reduced practice states. These states place some limitations on NP practice. In other words, the NP has partial autonomy.
This category is defined by the American Association of Nurse Practitioners (AANP) as states placing restrictions on NP autonomy in at least one of the following ways:
State law requires a career-long regulated collaborative agreement with another health provider in order for the NP to provide patient care, or
State law limits the setting of one or more elements of NP practice.
For example, the state may require an NP have an agreement with a collaborating physician, or practice with supervision for a certain number of hours before gaining full authority. There may be limits on prescribing or performing certain services independently. Or, a proximity requirement may mandate a collaborating physician be physically present during some of the NP’s hours or located within a certain mile radius of the NP’s practice.
While these limits impact NP independence, NPs in these states still contribute significantly to expanding access to care. See our list below for some of the nuances of NP autonomy in these states, and check with the state nursing board for full details.
Reduced Practice States List
Alabama
Alabama has proximity requirements for collaborating physicians. If the NP has less than 2 years (4,000 hours) experience, a physician must be physically present for at least 10 percent of the NP’s scheduled hours. This requirement eases to quarterly once an NP has 2 years (4,000 hours) of experience. Remote practice sites have to be visited by the physician at least twice per year.
Arkansas
NPs in Arkansas can gain full practice authority after completing 6,240 hours of experience under a physician’s authority. Arkansas also has proximity requirements for these collaborating physicians. The physician must be actively practicing medicine in the State of Arkansas or in a bordering county of another state.
Illinois
To obtain a full practice authority license, Illinois NPs must first have a collaboration agreement with a physician and complete 4,000 hours of clinical experience under the physician’s supervision. Even when practicing independently, NPs are limited in prescribing certain narcotics except in collaboration with a physician and reporting under the state’s Prescription Monitoring Program.
Indiana
Indiana NPs must have a collaboration agreement on file with a supervising physician. The physician cannot supervise more than two advance practice clinicians at a time.
Kentucky
Kentucky NPs can practice independently, but they must have collaborative agreements in place in order to prescribe medications. There is no requirements for proximity, chart reviews, or direct supervision. There are also no restrictions on how many NPs a physician can supervise at a time.
Louisiana
In Louisiana, NPs are required to have collaborative practice agreements (CPAs) in place in order to practice. There is no proximity requirement, but the physician must be available to communicate with the NP at all times. For this reason NPs may need a “back-up” physician in case their main collaborating physician is unreachable.
Mississippi
NPs in Mississippi are required to have a collaborating physician who reviews 10% of patient charts each month—or 20 total, whichever is less. The supervising physician must be within a 75-mile radius of the nurse’s practice location and meet with the nurse practitioner quarterly.
New Jersey
In New Jersey, NPs can practice independently, but they must have collaborative agreements in place with a physician to prescribe.
Ohio*
NPs in Ohio who want to practice independently need a collaboration agreement with a physician in place. NPs must have 500 hours of onsite supervision by a physician before having full prescriptive authority. Physicians in Ohio can supervise a maximum of five APCs at a time.
Pennsylvania
Pennsylvania requires NPs to have written collaboration agreements with two physicians - a primary and substitute. The agreement must cover protocols, a schedule for the physician’s analysis of the NP’s patient charts, and the specific rights and responsibilities of the two parties.
West Virginia*
West Virginia NPs may practice independently, but have a collaboration agreement with a physician or APRN in order to prescribe. NPs with a CNP, CNS, CNM, or CRNA credential may apply for full prescriptive authority after completing two years practice under the collaborative agreement.
Wisconsin
NPs in Wisconsin are required to have a collaborating agreement with a physician in order to provide pharmacologic-related care.
Nurse Practitioner Restricted Practice States
States with restricted practice authority place substantial limitations on NP autonomy. In other words, the NP must work under a supervising physician for their entire scope of practice. While the NP may have extensive autonomy in some clinical functions, they are not independent.
The AANP defines restricted practice authority as practice and licensure laws restricting the ability of NPs to engage in at least one element of NP practice. For example, state law may require career-long supervision, delegation, or team management by another health provider in order for the NP to provide patient care.
Some people believe these restrictions hinder the ability of NPs to fully meet the healthcare needs of their communities. Efforts are ongoing, however, to expand NP scope of practice and remove barriers, recognizing the immense value NPs bring to the healthcare system. Some restricted states have recently passed legislation to loosen restrictions as the NP gains experience.
See our list below for some of the nuances of NP restrictions in these states, and check with the state nursing board for full details.
Restricted Practice States List
California*
NPs who have completed 4,600 hours or three years of full-time clinical practice in California can apply for authority to work without contractual physician supervision, but only in facilities where at least one doctor or surgeon also practices. After working another three years in that practice setting, they can apply for full practice authority, without any setting restrictions.
Florida
NPs in Florida who have completed 3,000 hours under physician supervision in the last five years can now apply for an unrestricted license. Florida permits NPs to practice independently without physician supervision, but only in primary care settings.
Georgia
Georgia’s laws require NPs to have a protocol agreement with a supervising (or delegating) physician. The supervisory physician delegates authority to perform specific medical tasks such as ordering diagnostic tests and prescribing medications. NPs with prescriptive authority must have their charts reviewed by the delegating physician and see their patients quarterly. Supervising physicians can only supervise four NPs with prescriptive authority at a time.
Michigan
Michigan NPs don’t have the authority to practice independently. They must be supervised by a licensed physician. An NP’s tasks and functions must be delegated by a physician. NPs also are not recognized as primary care providers in Michigan.
Missouri
Missouri NPs are required to work with a collaborating physician to provide care. There is a proximity requirement that the physician be within 75 miles of the NP’s practice setting. An NP cannot apply for prescriptive authority until reaching 1,000 hours of experience. The physician must be immediately available for consultation at all times, either personally or via telecommunications. The collaborating physician must also review the work and records of the NP at least once every 2 weeks.
North Carolina
North Carolina NPs are required to have a collaborative practice agreement with a physician to provide care. The physician must be continuously available for consultation, collaboration, referral, and evaluation.
Oklahoma
In Oklahoma, NPs can practice independently. However, they are not allowed to prescribe medications and treatments without first entering into a supervisory agreement with a physician. Physicians are only permitted to supervise six NPs at one time.
South Carolina
NPs in South Carolina must have a practice agreement with a physician in order to practice and obtain prescriptive authority. The collaborating physician must be located within the state. If the physician is out of state, the NP must have an alternate in order to practice. Physicians are only permitted to supervise six NPs at one time.
Tennessee
In Tennessee, an NP must have a physician collaborator to provide care and prescribe. The supervising physician must be available for consultation at all times, or an alternate physician must be available. Chart reviews are mandatory (20% of charts) and the physician must visit remote sites where the NP practices monthly.
Texas
Texas NPs can only practice and prescribe under the supervision of a physician within a 75-mile radius. The physician must review 10% of the NP's patient charts randomly each month. NPs do not have authority to prescribe Schedule II substances. Physicians can only delegate prescriptive authority to seven nurse practitioners at one time.
Virginia
Newly licensed NPs in Virginia are required to have a collaborative agreement with a supervising physician. NPs can apply to practice independently once they have an equivalent of two years (for CNPs) or 1,000 hours (CNMs) practice experience with a collaborating physician.
Stay on Top of Changing Regulations with Zivian Health
Nurse practitioners play a vital role in meeting the healthcare needs of communities across America. The scope of practice for NPs varies from state to state, and full practice authority states are generally the best states for nurse practitioners’ who want independence.
That said, NPs in reduced or restricted states can also build fulfilling careers. No matter which state(s) you practice in, quality collaborations can bring immense value to your clinical practice.
How Zivian Health Supports Nurse Practitioners
If you are in need of a collaborating physician, Zivian Health is here for you. We connect nurse practitioners to a nationwide network of experienced physicians to form long-term, compliant healthcare collaborations. Finding you an excellent collaborator is where we begin, but our one-of-a-kind platform manages all the elements of collaboration compliance and quality so that you can focus on patient care.
The Zivian Health platform offers collaboration agreement storage, secure messaging and chart review features, a continually updated database of state regulations for Physician-APP collaborations, and creates an audit trail for all collaboration activity.
Connect with our team and get started today!
Note: The material contained in this is informational only and is not considered practice, financial, accounting, legal or other professional advice. State regulations regarding collaborative practice are subject to change. Always check with your state legislature, nursing or medical board to confirm regulatory information.
Sources & Data
https://www.aanp.org/advocacy/state/state-practice-environment
https://www.aanp.org/practice/practice-information-by-state
https://www.nursingworld.org/globalassets/docs/ana/ethics/principles-aprnfullpracticeauthority.pdf