
The corporate practice of medicine has a long history and is subject to varied interpretations and regulations across different states across the US.
This post provides an overview of the corporate practice of medicine, shedding light on its historical roots, legal underpinnings, financial implications, and variations that exist from state to state.
What Is the Corporate Practice of Medicine?
At its core, the corporate practice of medicine refers to the idea that the practice of medicine should be governed by individuals with clinical expertise rather than commercial or corporate entities.
This principle is grounded in the belief that physicians, as trained and licensed professionals, should have autonomy in medical decision-making to ensure the best interests of patients. The concept aims to protect the integrity of the doctor-patient relationship, emphasizing that medical decisions should be based on clinical judgment rather than financial considerations.
The corporate practice of medicine prohibition, a legal doctrine in many jurisdictions, serves as a safeguard against the potential exploitation of medical services for profit-driven motives. While the specifics vary, these prohibitions generally prevent non-physicians or corporate entities from directly employing physicians.
However, exceptions exist, allowing for various organizational structures that enable collaboration between healthcare professionals and corporate entities.
Historical Foundations
The origins of the corporate practice of medicine can be traced back to the early 20th century when the medical profession sought to protect its autonomy and shield the doctor-patient relationship from potential commercial exploitation. This principle emphasizes that medical decisions should be made by those with clinical expertise rather than influenced by profit-driven motives.
Historically, physicians operated as independent practitioners, running their practices and making medical decisions autonomously. However, as healthcare evolved, so did its organizational structures.
The rise of large healthcare systems, hospital affiliations, and corporate entities entering the healthcare arena marked a shift in the landscape of medical practice.

Legal Framework
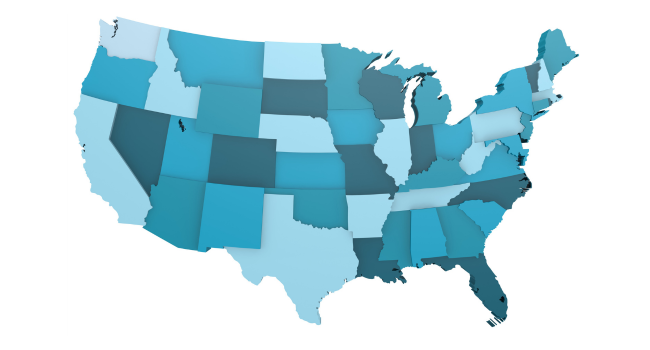
The legal framework surrounding the corporate practice of medicine is not uniform across the United States. Instead, it is a patchwork of state-specific regulations, each with its own nuances and exceptions.
The overarching goal of these regulations is to prevent non-physicians from interfering with medical decision-making and to maintain the professional independence of physicians.
Corporate Practice of Medicine Prohibition
Many states have what is known as a “corporate practice of medicine prohibition.” These laws generally prevent corporations or non-physician entities from employing physicians directly. The rationale behind such prohibitions is to safeguard the integrity of medical decision-making and protect patients from potential conflicts of interest.
However, each state has its own set of rules governing these practices. Some states have strict prohibitions, while others have carved out exceptions or created specific legal structures that allow for certain corporate arrangements involving physicians.
New Legal Structures Surrounding Corporate Practice of Medicine
Physician-Hospital Organizations (PHOs) and Management Services Organizations (MSOs) are examples of legal structures that have emerged to navigate these regulations.
PHOs allow physicians and hospitals to collaborate while maintaining certain legal and financial distinctions, and MSOs provide administrative services to physician practices without interfering with clinical decision-making.
To understand the corporate practice of medicine fully, it’s crucial to delve into the specifics of each state’s laws and regulations.
State-by-State Variations
The legal framework surrounding the corporate practice of medicine varies significantly across states in the U.S., reflecting the diverse approaches taken by different jurisdictions to address the intersection of healthcare and commerce.
While some states have stringent prohibitions to maintain the independence of physicians, others have adopted more flexible regulations that allow for certain corporate structures.
Prohibition States
In states with robust corporate practice of medicine prohibitions, non-physician entities are generally restricted from employing physicians directly. These laws aim to uphold the autonomy of physicians in clinical decision-making and prevent the undue influence of corporate interests.
California is a notable example of a prohibition state, where the Business and Professions Code explicitly prohibits the corporate practice of medicine.
Corporate Practice Permitted States
On the other end of the spectrum, some states have fewer restrictions on the corporate practice of medicine. In these states, non-physician entities may employ physicians directly, leading to various organizational models such as physician-hospital organizations (PHOs) and management services organizations (MSOs).
Texas is an example of a state where the corporate practice of medicine is generally permitted, though certain restrictions and requirements may apply.
Intermediate States
Between the prohibition and permissive states, there are states with intermediate regulations that allow for specific corporate arrangements under certain conditions. These conditions may include maintaining the professional autonomy of physicians, ensuring that medical decisions are not unduly influenced by financial considerations, and providing transparency to patients.
Florida exemplifies an intermediate state with regulations that permit certain corporate structures while imposing limitations to protect against potential abuses.
These examples illustrate the diversity of approaches among states, highlighting the need for healthcare organizations and professionals to navigate a complex legal landscape with a keen awareness of state-specific regulations.
Navigating the Landscape
The Corporate Practice of Medicine is part of the much larger landscape of modern healthcare. Below are areas where the Corporate Practice of Medicine plays a role.

Financial Implications
The financial landscape of healthcare has undergone significant transformation in recent decades, with the corporate practice of medicine playing a central role. The financial implications of these arrangements can vary widely depending on the legal and regulatory environment of each state.
Physician Employment
One prominent trend is the increasing employment of physicians by hospitals and health systems.
This shift from independent practice to employment has financial implications for both physicians and healthcare organizations. Physicians may benefit from greater financial stability, including a steady salary, benefits, and reduced administrative burdens.
On the other hand, healthcare organizations may achieve operational efficiencies, improved coordination of care, and enhanced negotiation power with payers.
Integration of Services
Corporate practice arrangements often involve the integration of various healthcare services. This integration can lead to economies of scale, improved resource utilization, and enhanced patient care coordination.
Integrated models may involve the consolidation of medical practices, diagnostic services, and ancillary services under a single corporate entity.
Financial Pressures
While corporate practice arrangements offer potential financial benefits, they also introduce new challenges.
Financial pressures within a corporate structure may influence medical decision-making, potentially leading to over-utilization of services, unnecessary procedures, or a focus on revenue generation rather than patient outcomes.
Balancing financial imperatives with ethical considerations remains a constant challenge in the evolving landscape of healthcare delivery.

Patient Impact
At the heart of the corporate practice of medicine is its impact on patient care. Patients are directly affected by the structure and functioning of the healthcare system, and variations in state regulations can shape their experiences in significant ways.
Access to Care
Corporate practice arrangements have the potential to enhance access to care by creating more streamlined and coordinated healthcare delivery systems.
Through integrated services and collaborative models, patients may experience improved access to a range of medical services, from primary care to specialized treatments.
Quality of Care
While financial considerations can impact the quality of care, they are not inherently detrimental. Integrated healthcare systems can lead to improved care coordination, reduced duplication of services, and better management of chronic conditions.
However, when financial motives supersede clinical judgment, there is a risk of compromising the quality of care. Striking the right balance is crucial to ensure that patients receive high-quality, evidence-based care.
Patient Choice
The consolidation of healthcare entities can raise concerns about reduced competition and limited patient choice. In some regions, patients may find themselves with fewer options for healthcare providers, potentially limiting their ability to choose based on preferences, quality metrics, or cost considerations.

Technological Advancements
Technological innovations play a pivotal role in shaping the corporate practice of medicine. Electronic Health Records (EHRs), telemedicine, data analytics, and other digital tools have the potential to enhance patient care, improve efficiency, and facilitate collaboration among healthcare professionals.
EHR Integration
The adoption of electronic health records is a key component of many corporate practice arrangements. EHRs enable seamless sharing of patient information among different healthcare providers within a corporate entity.
This integration supports better-informed medical decision-making, reduces the likelihood of medical errors, and enhances overall patient care.
Telemedicine
Rapid growth of telemedicine has further transformed how healthcare is delivered, especially in the context of corporate practice. Telemedicine allows patients to access medical services remotely, expanding the reach of healthcare providers and improving patient convenience.
However, regulatory nuances in telemedicine vary from state to state, adding an additional layer of complexity to corporate practice arrangements.
Data Analytics
Data analytics and artificial intelligence are increasingly used to derive insights from large datasets, facilitating evidence-based decision-making and personalized patient care.
These technologies can be leveraged within corporate structures to identify trends, predict patient outcomes, and optimize resource allocation.
Conclusion
In conclusion, the corporate practice of medicine stands at the crossroads of tradition and innovation, ethics and economics. Understanding its historical foundations, legal framework, financial implications, and ethical considerations is crucial for healthcare professionals, organizations, and policymakers alike.
As we navigate the complex terrain of modern healthcare, striking the right balance between business imperatives and patient-centered care remains an ongoing challenge—one that requires continuous dialogue, adaptation, and a steadfast commitment to the principles that define the noble profession of medicine.